New treatments for the eye disease that can take lives as well as vision
By: Alan L. Wagner, MD and Kapil G. Kapoor, MD
It’s well known that skin cancer is the most common of all cancers, and that melanoma, which accounts for only two percent of these cancers, causes a large majority of skin cancer deaths. Over the past twenty years, those cancers and deaths have increased between three and five-fold. It’s less well recognized that there has been a similar increase in the incidence of melanoma of the eye and in its sequelae: from loss of vision to loss of life. Approximately 50 percent of patients with choroidal melanoma (also called uveal melanoma) will develop metastasis by 10 to 15 years after diagnosis.
 These tumors are rare, and while we don’t know the exact cause, we do know that individuals with red hair, fair skin and blue or green eyes are at higher risk; as, of course, are those with a family history of skin conditions like dysplastic nevus syndrome.
These tumors are rare, and while we don’t know the exact cause, we do know that individuals with red hair, fair skin and blue or green eyes are at higher risk; as, of course, are those with a family history of skin conditions like dysplastic nevus syndrome.
As with most cancers, early detection means safer, more effective treatment, and therein lies the challenge: in its earliest stages, choroidal melanoma is relatively symptom-free. The tumor doesn’t cause pain or discomfort, and there are few visual cues. By the time the patient experiences symptoms, the disease is usually more advanced. These include blurred vision, flashing lights or shadows – the same symptoms that often beset patients over the age of 40.
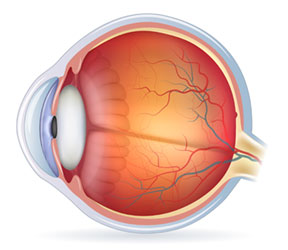
Most melanomas in the eye are diagnosed during a dilated eye exam, using an ophthalmoscope and slit lamp. It’s usually at this point that we see the patient, and we begin by measuring the tumor(s) with our unique scanning laser and camera that records in multiple wavelengths. We perform angiography, and when indicated, follow with CT, MRI or even PET imaging. It’s critical to determine at the outset whether the melanoma has metastasized.
Once the diagnosis is confirmed, we work collaboratively with the excellent local oncologists to determine the best course of treatment for each individual patient. Today’s modalities offer hope where little to none previously existed for eradicating the tumor, improving survival, and preserving sight.
For certain small tumors, we use transpupillary thermal therapy – TTT – a method of delivering non-ionizing radiation to the tumor, using a near-infrared laser, killing the cancer cells without harming the eye. If that fails to work, and for larger tumors, we use a form of brachytherapy, placing a small plaque embedded with radioactive seeds against the outside of the eye. The patient is then patched for five days before plaque removal. We’ve seen success in killing the tumors with this method in over 85 percent of cases.
Today, we’re able to do genetic testing that can help us more accurately determine a patient’s prognosis. Certain genetic mutations confer increased susceptibility to uveal melanoma metastasizing. There is ongoing and very exciting research and clinical trials being conducted in our clinic and others across the country that patients are being enrolled in if they’re found to have higher risk changes, or if they show metastatic disease. Three or four years ago, we had nothing to offer these patients. Today we can gather much more information to help us determine the appropriate follow up and care.
Perhaps the most crucial message for patients is the importance of the annual, dilated eye examination. And because of the potential for conversion, the importance of close follow up cannot be overstated. If uveal melanoma is caught early and treated when the lesion is small, there are well-tolerated modalities that can save their vision – and their lives.
 Alan L. Wagner, MD, FACS founded the Wagner Macula & Retina Center in 1987. He completed medical school at Vanderbilt University School of Medicine, residency at EVMS and a fellowship at Weill Cornell University Medical Center.
Alan L. Wagner, MD, FACS founded the Wagner Macula & Retina Center in 1987. He completed medical school at Vanderbilt University School of Medicine, residency at EVMS and a fellowship at Weill Cornell University Medical Center.
 Kapil G. Kapoor, MD completed medical school at Ohio State University, residency at the University of Texas Medical Branch-Galveston and a fellowship at The Mayo Clinic.
Kapil G. Kapoor, MD completed medical school at Ohio State University, residency at the University of Texas Medical Branch-Galveston and a fellowship at The Mayo Clinic.
Both are Board-certified ophthalmologists specializing in vitreoretinal surgery. www.wagnerretina.com.

